Increased intracranial pressure - Pediatric OSCE and cases
The post outlines the topic of raised intracranial pressure (ICP) in children. This includes definition criteria, physiological considerations such as cerebral perfusion pressure (CPP), causes, Intracranial pressure monitoring, and treatment of intracranial hypertension. Keep scrolling!
Table of Contents
Physiologic Considerations
Normal values
The normal range for ICP varies with age. Values for children are not well established when compared to adults. Usually, normal limits are taken as 5 to 15 mm Hg
- < 10 to 15mmHg for adults and older children
- 3 to 7 mm Hg for young children
- 1.5 to 6 mm Hg for term infants.
- ICP can be sub-atmospheric in newborns.
Definition of Intracranial hypertension
Current pediatric data support an ICP >20 mm Hg as a threshold to define intracranial hypertension requiring treatment. Sustained ICP values of greater than 40mm Hg indicate severe, life-threatening intracranial hypertension.
A surge in ICP normally occurs with activities such as suctioning, painful stimuli, and coughing and does not warrant intervention unless it does not return to baseline within 5 minutes. It is important to distinguish “normal” or expected increases/spikes in ICP while considering the treatment, therefore the word sustained rise in ICP is very important.
Cerebral Pressure Dynamics
Monro-Kellie doctrine
Intracranial pressure is the sum total of pressure exerted by the brain, blood, and cerebrospinal fluid (CSF) in the non-compliant cranial vault.
The Monro-Kellie doctrine states that the sum of the intracranial volume of the brain (» 80%), blood (» 10%), and cerebrospinal fluid (» 10%) is constant.
An increase in any one of these components must be offset by a decrease in another to keep the total volume constant or else the ICP will increase.
In response to increases in intracranial volume initial compensation occurs by
- Displacement of CSF from the ventricles and the cerebral subarachnoid space to the spinal subarachnoid space (vertebral canal),
- Decreased production of CSF, and
- Increased absorption of CSF.
- Infants and children with open fontanels and sutures may be able to compensate better but will still be susceptible to acute increases in ICP.
Compliance
Compliance is an indicator of the brain’s tolerance to increases in ICP. Each patient has varying degrees of compliance even with similar injuries.
When the patient’s compliance is exhausted, there is a dramatic increase in the pressure/volume curve, leading to a rapid elevation in ICP.
Cerebral Blood Flow
In an uninjured brain, cerebral blood flow CBF) is regulated to supply the brain with adequate oxygen and substrates.
CBF in excess of tissue demand leads to hyperemia and increased ICP. This
Certain physiologic factors like hypercarbia, acidosis, and hypoxemia cause vasodilatation, leading to increased CBF.
Seizure activity and fever will increase cerebral metabolic rate and CBF. This is the reason why methods to decrease the cerebral metabolic rate, such as hypothermia and barbiturates, will decrease CBF and thus the ICP.
Cerebral perfusion pressure
Cerebral perfusion pressure (CPP) is the pressure at which the brain is perfused. It is an important indicator of cerebral blood flow.
Thus CPP provides an indirect measurement of the adequacy of CBF.
It is calculated as
CPP = (MAP – ICP)
Where MAP is mean arterial pressure (MAP) which equals = 1/3 systolic pressure + 2/3 diastolic pressure and ICP is intracranial pressure.
A reduction in CPP can occur from an increase in ICP, a decrease in blood pressure, or a combination of both factors.
Normal CPP values
- Adults >70 mm Hg
- Children >50–60 mm Hg
- Infants/toddlers >40–50 mm HgCPP
< 40 mm Hg is a significant predictor of mortality in children with TBI.
Cerebral Autoregulation
Cerebral autoregulation maintains a steady cerebral blood flow (CBF) within a CPP range of 50-150 mmHg by vasoconstriction and vasodilatation of the cerebral vessels during the fluctuations in systemic blood pressure. For eg. in systemic hypertension or hypotension (states of shock)
These mechanisms of Autoregulation are lost at CPP values less than 50 mmHg. Once autoregulation is lost, CBF and cerebral blood volume (CBV) become dependent on changes in systemic blood pressure.
Major mechanism causing raised ICP

- An increase in the volume of the brain for eg. Cerebral edema.
- Space occupying lesion eg. Intracranial tumor or Intracranial bleed.
- Abnormal increase in CSF volume, either production or obstruction. eg. hydrocephalous.
These mechanisms can operate singly or in combinations.
Causes of Intracranial Hypertension
Intracranial (primary)
- CNS infections – meningitis, encephalitis, brain abscess, cerebral malaria, neurocysticercosis.
- Trauma such as epidural and subdural hematoma, cerebral contusions, and edema.
- Brain tumor
- Intracranial bleeding – intracerebral and intraventricular hemorrhage.
- Others – ischemic stroke, hydrocephalous, idiopathic or benign intracranial hypertension.Status epilepticus.
Extracranial (secondary)
- Hypoxic Ischemic Injury - airway obstruction, hypoventilation, shock.
- Metabolic – hyperpyrexia, hepatic failure, lead intoxication.
- Drugs such as tetracycline, rofecoxib
- Others – hypertensive encephalopathy
Postoperative
- Mass lesion (hematoma)
- Cerebral edema
- Increased cerebral blood volume (vasodilation)
- CSF obstruction.

Vasogenic cerebral edema vs Cytotoxic cerebral edema
Vasogenic cerebral edema is due to injury to the blood-brain barrier and increased capillary permeability around the area of injury or inflammation, particularly in CNS infections. It can be local or diffuse and occurs around mass lesions and inflammatory processes e.g., meningitis, encephalitis).
Cytotoxic cerebral edema or Cellular swelling occurs following cerebral ischemia and hypoxia causing irreversible cell damage and death. Osmolar swelling may occur because of increased local osmolar load around necrotic foci caused by infarction or contusion, and possibly because of increased cerebral blood volume (hyperemia) in CNS infections.
Patients with cerebral edema may have a combination of all 3 mechanisms of raised ICP operating. When the primary cause of increased ICP is intracranial, normalization of ICP depends on rapidly addressing the underlying brain disorder. Intracranial hypertension due to an extracranial or systemic process is often remediable.
Intracranial hypertension in traumatic brain injury
Following traumatic brain injury (TBI), intracranial hypertension is multifactorial and may involve
- Cerebral edema
- Hyperemia due to loss of autoregulation
- Hypoventilation leading to hypercarbia and consequently cerebral vasodilation
- Hydrocephalus resulting from obstruction of the CSF pathways or its absorption
- Increased intrathoracic or intra-abdominal pressure as a result of mechanical ventilation, posturing, agitation, or Valsalva maneuvers.
A secondary increase in the ICP is often observed 3 to 10 days after the trauma mainly as a result of a delayed formation of epidural or acute subdural hematoma, traumatic hemorrhagic contusions with surrounding edema, sometimes requiring evacuation. cerebral vasospasm, hypoventilation, hyponatremia
Intracranial Pressure Monitoring
Indications
- Patients with GCS of 8 or less
- Patients with TBI who have an abnormal admission head CT scan.
- Patients with a GCS greater than 8 also might be considered for ICP monitoring if they require a treatment that might increase ICP such as positive end-expiratory pressure(PEEP).
- Other, less common indications include
- Patients with multiple systemic injuries with altered level of consciousness and subsequent to removal of an intracranial mass e.g., hematoma, tumor.
- Must be considered in nontraumatic conditions in which an intracranial mass lesion is present e.g., cerebral infarction) and has a likelihood of expansion leading to intracranial hypertension and clinical deterioration.
The duration of monitoring is until ICP has been normal for 24 to 48 hours without a need for therapy to reduce ICP.
Intracranial pressure waveforms
The normal ICP waveform contains three phases

- P1 (percussion wave) represents arterial pulsations.
- P2 (rebound wave) reflects intracranial compliance.
- P3 (dichrotic wave) represents venous pulsations
Treatment of raised ICP
Goals of therapy

- Maintain ICP less than 20 to 25 mm Hg.
- Maintain adequate CPP usually greater than 60 mm Hg, by maintaining adequate MAP.
- Avoid factors that aggravate or precipitate elevated ICP.
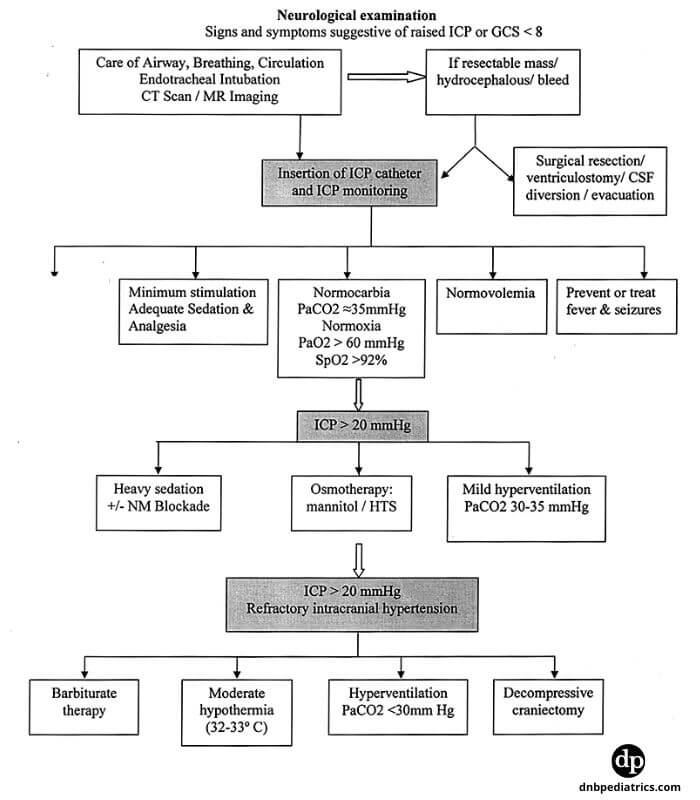
Algorithm for the treatment of raised ICP
Treatment Systemic Hypertension
Elevated blood pressure is seen commonly in patients with raised ICP. Characteristically SBP increase is greater than DBP. It is unwise to reduce elevated blood pressure associated with untreated raised ICP, especially in patients with intracranial mass lesions, because high blood pressure maintains cerebral perfusion.
Sympathomimetic-blocking antihypertensive drugs, such as beta-blocking drugs labetalol, esmolol, or central-acting alfa-receptor agonists clonidine, are preferred because they reduce blood pressure without affecting the ICP.
Agents with a short half-life have an advantage when the blood pressure is labile. Systemic hypertension may resolve with sedation. If the decision is made to treat systemic hypertension, vasodilating drugs, such as nitroprusside, nitroglycerin, and nifedipine, should be avoided; these increase ICP, which may be deleterious to the marginally perfused injured brain.
Treatment of anemia
Maintain optimal hemoglobin concentration around. A restrictive transfusion threshold is recommended since volume expansion may further ad to raised ICP.
Author

Ranjith C S. | DNB (Pediatrics), DM (Medical Oncology)
Ranjith has completed Pediatric Residency from Kanchi Kamakoti Childs Trust Hospital and further trained in Medical Oncology from JIPMER
2 comments
🩺 Help us refine this article — share corrections or additional information below. Let's elevate the accuracy of knowledge together! 💉💬