Understanding Physiology and Mechanics of Pediatric ECG
The invention of ECG - Timeline
- 1843 Emil Du Bois-Reymond, a German physiologist, described "action potentials" of muscular contraction using a galvanometer.
- 1887 The English physiologist Augustus Waller, defined and demonstrated the first human electrocardiogram.
- 1906 Einthoven assigned the letters P, Q, R, S, and T to various deflections, described the electrocardiographic features of cardiovascular disorders.
- 1938 The AHA and the Cardiac Society of Great Britain defines the standard positions and wiring, of the chest leads V1 - V6. The 'V' stands for voltage.
- 2018 – Smartphone 12‐lead ECG. Lindow et al 2018
- What's next - 80 lead ECG?
Relevant Physiology for understanding ECG
Heart Muscle
- The center of physiology is a very special muscle comprising of myocytes. It strikingly differs from the skeletal muscle.
- It never tire's out due to many more mitochondria as compared to other muscles
- It keeps Contracting and relaxing in repetition and rhythm.
- ATP's for functioning is primarily produced via aerobic metabolism
4 Characteristic features of cardiac muscles
1. Involuntary action
Cardiac muscle can Generate and transmits electrical impluse on their own. They are connected by cytoplasmic bridges or syncytia, so as, if one is activated, the depolarization spreads to adjacent cells.
2. Intrinsic control
Controlled by the autonomic nervous system
3. Unique structure
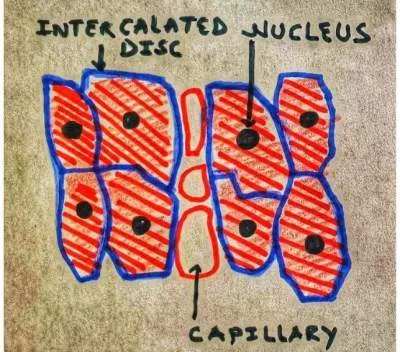
Cardiac muscles are striated and branched just like skeletal muscles, But they are shorter, possess numerous mitochondria ( which makes them foolproof from fatigue). They have a single nucleus. The fibers are connected via an intercalated disc which has Gap junction and Desmosome.
What does Gap junction do?
It allows cardiac muscles to contract in synchrony by allowing rapid transmission of electrical activity
What does Desmosome do?
A desmosome holds the ends of cardiac muscle fibers together. When the muscle fibers are contracting, the cells pull apart due to stress. Desmosome helps in avoiding this.
4. Pacemaker cells
- These are modified myocytes, they do not have organized sarcomere.
- The electrical impulse is generated by the Pacemakers cell, explained below in detail.
- Note - they do not contribute to contractile force and intensity. (No organized sarcomere)
Unusual channels in pacemaker cells that are permeable to both Na + and K+ (If or funny channels)
↓Unstable resting membrane potential (- 60mV. )
↓Membrane potential never rests, hence pacemaker cells
Generation of Cardiac rhythm
- Cardiac myocytes are capable of self-excitation and relaxation at their own pace and rhythm without input from the nervous system. (discussed above)
- Amongst these, the SA node can generate action potentials at a relatively higher rate than other pacemaker cells, therefore leading the process under normal circumstances and overriding other impulses.
- Trigger for contraction is called cardiac excitation-contraction coupling mediated through the movement of Na, K, and Ca, in and out of cells.
- The pathologies where SA node cannot function normally, cardiac contraction may be initiated by others like AV node or even ventricles. Such rhythms are called escape rhythms.
What affects the functionality of the SA node?
The following things alter the heart rate by affecting the SA node
1. Nervous control
- Vagus nerve (Parasympathetic control), which slows the heart rate.
- Spinal nerves from T1 to T4 (sympathetic control) – which increase heart rate and contractility.
2. Electrolytes
Major determining electrolytes are K followed by Calcium. Hyperkalaemia can cause severe bradycardia while hypokalaemia can cause tachycardia.
3. Hypoxia and hypercarbia
Hypoxia can cause severe bradycardia. While hypercarbia can cause initial tachycardia followed by bradycardia.
4. Drugs
Drugs can change HR by affecting the SA node, AV node, or ventricular myocytes.
- Negative chronotropic - Drugs can reduce heart rate eg. beta-blockers and CCB's.
- Positive chronotropic - Drugs can increase heart rates Such as dopamine and dobutamine.
- Negative inotropy - decrease in contractile force eg. beta-blockers, calcium channel blockers, and some anti-arrhythmic drugs eg. flecainide and disopyramide.
- Positive inotropy - increase contractile force. eg. dopamine and dobutamine.
Conduction of Rhythm
Network of transmission
The network consists of 3 main pathways
- Conducting cells: These are found in The atrioventricular (AV) node, The bundle of
- His and bundle branches, The Purkinje fibers
- Contractile cells: These form the main cell type in the atria and ventricles.
What is responsible for the transmission of the action potential?
Cardiac myocytes are connected by an intercalated disc. Refer to image 1. These discs have - Gap junctions, adhering junctions, and desmosomes. Gap junction help in the electrical coupling of the cardiac muscle so that the impulse can spread as fast as possible and cells can beat in synchrony. This is called electrical coupling.
The disc allows them to contract in synchrony by allowing rapid transmission. They have a single nucleus. Pacemaker cells (see above), located in the SA node on the wall of RA generate rhythm which spread through the gap junction in the intercalated disc to other myocytes.
How does the ECG machine works
What is recorded?
Electrical activity arising from heart muscle is recorded. But while doing so the activity
of other muscles is also recorded. The machine tries to filter these.
How it is recorded?
With each depolarization and repolarization, the electrical activity from the heart spread around by simple conduction. To pick up this, the array of sensors, officially called leads are placed strategically to cover the heart's activity as a whole.
ECG leads system
Standard limb leads also called bipolar leads, use one positive and one negative electrode. Chest lead or Unipolar leads also called augmented leads use only one positive electrode ( they use other electrodes as a negative point).
The leads are connected to a device that measures potential differences between these electrodes and when all the leads are measured simultaneously, the resulting graph is an electro-cardiogram.
An ECG machine uses the information it collects via its four limb and six chest electrodes to compile a comprehensive picture of the electrical activity in the heart as observed
from 12 different viewpoints, and this set of 12 views or leads gives the 12-lead ECG
its name.
Why some waveforms are smaller and why some are bigger in ECG?
The voltage changes detected by ECG machines are very small, as small as millivolts. The size of each wave corresponds to the voltage generated by the event that created it. Higher the voltage, the larger the ECG wave.
How does ECG tells the duration of events like depolarization or repolarization?
The ECG paper moves at a constant rate of 25 mm/s. This is standardized. Each small (1 mm) square on the ECG represents 0.04 s, and each large (5 mm) square represents 0.2 s.
If the width of a particular wave is measured, the duration of the event causing it can be easily calculated. Knowing the normal ECG wave or interval durations and variations in children helps identify the deviation from normalcy.
The flow of electrical activity and deflection in ECG
When the electrical current flows toward a particular lead, the deflection at that lead will be positive. If it flows away from that lead, it will be negative.
Now if you know which lead is placed where it can easily determine the pattern. And based on normal pediatric ECG patterns, we can determine pathologies. Knowing the direction of electrical impulse determines which area or areas of the heart are affected.
Recording an ECG in child - OSCE station
This is a step-by-step guide on how to record an ECG in a child during an observed OSCE station.
| Preparation | Wash hands and use PPE as appropriate. Introduce yourself. Identify correct patient by name, DOB, hospital number, wrist band, etc Enquire about pain and discomfort beforehand |
| Consent | Gain verbal consent, explain what and why are you doing ECG, answer questions if asked. Obtain permission to expose part, offer parent/career/attendee to be with the child. |
| Preparing chest for leads | This is important for good results, expose adequately, take assistance if needed or when appropriate. May need to shave hair for good conduction in adolescent patients. May use alcohol wipe if leads not sticking. Avoid pressing hard, may damage the lead, and maybe uncomfortable for kids. |
| Prepare equipment | Enter patient demographic detail in the machine. Check correct date and time. Check paper speed settings |
| Pediatric ECG Lead placement | This will be discussed in detail in the next chapter but in summary. V1 - 4th intercostal space, right sternal edge V2 - 4th intercostal space, left sternal edge. V3 Midway in between V2 and V4 V4 5th intercostal space, mid- clavicular line V5 Left anterior axillary line, same horizontal level as V4 V6 Left mid-axillary line, same horizontal level as V4 and V5 Start attaching Red, yellow, Green, and Black (ride your green bicycle) leads in a clockwise direction starting from the right wrist Red electrode – right forearm, proximal to the wrist Yellow electrode – left forearm, proximal to the wrist Green electrode – left lower leg, proximal to ankle. Black electrode – right lower leg, proximal to the ankle |
| Recording ECG | Confirm all leads placed properly, request the child (if age appropriate) to stay still to avoid catch-up artifacts. Start recording. |
| Post recording | Remove leads gently, clean the part and or offer assistance |
| Counsel parents | Declare the procedure is over and the expected time the results will be available. |
| Labeling | Label the ECG appropriately with name, time, and DOB to ensure correct identification if not already recorded by the machine. Note any significant events during the procedure. |

This article is reviewed pre-publication
References
- Heart electrical activity. Emma Jakoi
- Muscle: Cardiac Muscle - The histology guide.
- Making Sense of the ECG: A Hands-On Guide, Fourth Edition
- Sinoatrial Node Action Potentials. CV Physiology
- Adult & Paediatric Resting Electrocardiography (ECG)- Queensland Health
Author

Parvez Patel | DCH, DNB (Pediatrics), FNB (Pediatric Cardiology), Advanced Fellow RACP
Parvez has completed Pediatric residency from LTMC Mumbai and is currently working as advance fellow in cardiology in Australia
💡 Join the Discussion!
🩺 Help us refine this article — share corrections or additional information below. Let's elevate the accuracy of knowledge together! 💉💬