Case scenarios | Pediatric OSCE stations
This guide includes practice OSCE stations based on case scenarios, data interpretation and image based diagnosis in pediatrics. Practicing OSCE stations helps in developing OSCE skills along with time keeping for final exams.
Station 1. Case-based scenario - Vision problem with recurrent infections
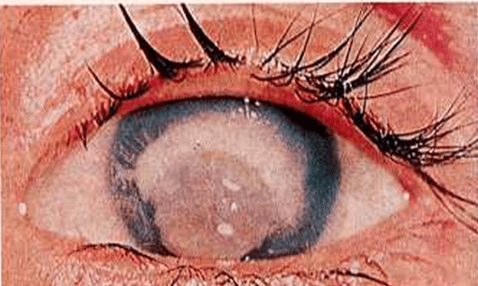
A 3-year-old girl child, with a weight of 7 kg and height of 75 cm, is brought with complaints of difficulty in vision and pain in the left eye with discharge. The child also has h/o recurrent episodes of loose stools and pneumonia. The examination findings are shown below.
Answer the following questions
- What is the diagnosis?
- Enumerate the WHO staging and mention what stage this child belongs to?
- What is the prognosis?
- How can this be prevented?
Answers
1. Vitamin A deficiency
2. WHO Stages
Primary signs
- X 1 A: Conjunctival xerosis
X 1 B : Bitot's spots - X2 : Corneal xerosis
- X3A : Corneal ulceration (<1/3rd)
- X3B : Keratomalacia
Secondary signs
- XN : Night blindness
- XF : Xerophthalmia fundus
- XS : Corneal scars
Child belongs to Stage X3B
3. Keratomalacia is usually irreversible and results in scar formation
4. Administer one dose of 1 lac units of vitamin A at 9 months followed by 4 more doses of 2 lac units each at 18, 24, 30 and 36 months. Consumption of Vitamin A rich food should be encouraged.
Station 2. Case-based scenario - Abdominal pain and weakness of lower limbs
14-Year-old female child presented with pain in the abdomen for the past 10 days. She also developed vomiting / loose motions for past 4 days and complaints of weakness in both lower limbs. She is unable to walk past 24 hours. On examination - she is hypertensive, tachycardia +++, has poor tone in both lower limbs, power grade 2 in both LL, DTR not elicitable. Answer the following questions.
- What could be 2 differential diagnoses?
- Investigations revealed Na – 110 / K 4, SGPT 37, the patient passed high colored urine - What is the probable diagnosis?
- Suggest one investigation for confirming diagnosis?
- How this could be treated?
Answers
- GBS / Acute intermittent Porphyria / Hypokalemia
- Acute Intermittent porphyria
- Urine for Porphyria (delta-aminolevulinic acid (ALA) and porphobilinogen (PBG))
- Avoid precipitating drugs. Medications- Hematin, and Panhematin is used to treat.
Station 3. Case scenario - Abdominal pain with rash
15 year old male presented with pain in abdomen for past 25 days which is acute intermittent and periumblical, he also developed swelling over scrotum 6 days back which subsided within 24 hours. Past 2 days the patient is having pain over right wrist with swelling of Rt knee. Patient also developed rash over gluteal region. Patient was passing red stool. Per abdominal examination showed an empty Rt lower quadrant. Take a look at the image and answer the following questions.

- Name probable diagnoses?
- What complication patient is shown in the Xray image?
- Medical treatment (specific for disease) for the diagnosis?
Answer
- HS Purpura
- Intussusception
- Steroids
Station 4. Case based scenario - Near drowning
A 4-year-old presented to ED with a history of near-drowning while playing in the pool. His vitals are stable but he is irritable and has respiratory distress. Answer the following questions.
- How do you differentiate Drowning from Near drowning
- List 3 predisposing aetiological factors for drowning.
- List 2 electrolytic disturbances and 1 hematological complication of near-drowning
- What is the commonest radiological finding?
Answers
1. Death within 24 hours of an immersion event is drowning while any survival from an immersion event is near-drowning
2. Predisposing factors can be Seizures, Long QT syndrome, and intoxication such as sedating drugs like cough suppressants.
3. Hypernatremia Hyperkalemia, Hypercalcemia, Hypermagnesemia, Hemolysis
4. Pulmonary edema
Station 5. Case-based scenario - difficult child with self stimulatory behaviour
Upon initial visit, a mother reluctantly tells you that her child, a 22-month-old female infant, recently has been diagnosed as autistic and has been referred to special education services by her previous physician.
Developmental history shows that she is sitting, hitching, walking, and running, but always on her knees. She is not socially interacting and has many self-stimulatory behaviors, such as arm flapping, rocking, and hand posturing. She says two words, "Mama" and "Dada", with the remainder of her vocalization consisting of high-pitched sounds. The mother claims her receptive language is good and that she points to body parts. The mother says that she can drink from a cup, but can't feed herself. On closer examination, you find that the mother must hold the cup as the child drinks from it.
Physical examination reveals a fair 22-month-old child, who avoids eye contact and dislikes touching, Wt is at 15%, Ht is at 15%, and HC is at 30%. Other than this, her examination appears to be WNL, although you note that a neuro examination is difficult due to her complete lack of cooperation.
What could be the diagnosis?
Answer
Missed phenylketonuria
Station 6. Case scenario - Chronic sinusitis and hematurea
A 12 year old female had a 2 year history of chronic sinusitis. She had episode of hemoptysis and respiratory distress. Urine analysis also reveals hematuria. Answer the following questions.
- What is the most likely diagnosis?
- What lab tests can help in diagnosing this patient
- Most important d/d for this patient
Answers
- Wagener granulomatosis
- ANCA, anti-PR3, Proteinase 3 – normally PR-3 is restricted to neutrophils granules but in this disease, they are on the neutrophil surface
- Churg-Strauss syndrome. Vasculitis- asthma, circulating eosinophilia, and eosinophils on skin biopsy. There is no destructive upper airway disease like in this case.
Station 7. Case scenario - Isolated Skin lesion
A 16-month-old girl has come to your outpatient practice for routine vaccination. During a routine examination, this raised skin lesion was seen above the left buttock. Answer the following question.

What is the diagnosis?
What treatment should be offered?
Answer
1. Capillary Haemangioma.
2. None for a haemangioma in this anatomical site.
Bit of theory
This is a haemangioma often called a strawberry naevus. These are not usually present at birth but develop in the first few weeks or months of life. They initially increase in size until 8 - 12 months and then regress.
By school age, most will have completely resolved. As there is a spontaneous resolution of these lesions no treatment is usually required. The exception is for cases where the position of the haemangioma causes functional problems. For example, if the lesion obscures the visual axis, treatment would be needed to allow normal visual development.
Station 8. Case scenario - Fever with lymphadenopathy
5-Year-old male child presents with a fever for the past 10 days. Fever is high grade, continuous in nature without chills and rigor. There are no associated loose motions, vomiting, headache, photophobia, cough, cold, or rash. On examination, the child is conscious, febrile, and normotensive. Conjunctiva is congested with no apparent discharge. Two cervical lymph nodes (Right-sided) are palpable, 2 cm approx each. There is desquamation of skin around the fingers. There is no hepatosplenomegaly . The rest of the systemic examination is normal. Answer the following questions.
- What is the most probable diagnosis?
- What characteristic feature can be found in complete blood counts?
- What is the most common cause of death in above- mentioned patient?
- What drug ( drug of choice ) you would like to give to this patient
Answers
- Kawasaki disease
- Thrombocytosis
- Congestive heart failure, coronary aneurism later
- Intravenous immunoglobin
Station 9. Case scenario - Delayed milestones and dyselectrolemia
A 10-month-old boy, weighing 3 kg has polyuria, polydipsia and delayed motor milestones. Investigations show blood levels of creatinine 0.5 mg/dL. potassium 3 mEq/L, sodium 125 mEq/L, chloride 88 mEq/L, calcium 8.8 mg/dL, pH - 7.46, and bicarbonate 26 mEq/L. Ultrasonography shows medullary nephrocalcinosis. Answer the following questions.
- What is the most likely diagnosis?
- What is the associated antenatal issue?
- What is the pattern of inheritance?
Answer
- Barter syndrome
- Polyhydramnios
- Bartter syndrome is inherited in an autosomal recessive manner, except for type 5, which is inherited in an X-linked recessive matter.
Bit of theory
Bartter syndrome is a group of rare genetic disorders with impaired kidney ability of the kidney to reabsorb salt which leads to various electrolyte abnormalities and fluid concentrations in the body.
The electrolytes affected are potassium, calcium, magnesium, sodium, and chloride. The symptoms and severity of Bartter syndrome vary from one person to another and can range from mild to severe.
Age of onset of ranges from before birth to adulthood. Treatment is aimed at correcting electrolyte imbalances through the use of supplements and medications such as nonsteroidal anti-inflammatories (NSAIDs) and diuretics.
Station10. Case scenario - Preterm with no verbal language
You have seen a 12-month-old child since birth. His neonatal history is significant for a premature delivery at 32 weeks of age, followed by a course of antibiotics in the NICU for presumed meningitis and hyperbilirubinemia requiring phototherapy.
Since discharge, he has thrived, with only multiple episodes of otitis media marring his course. On his 12-month physical examination, you find that he is not saying any words including "mama" or "dada". He does respond well to "pat-a-cake" and other baby games and to someone entering the room. He did coo, laugh, and babble at the appropriate ages, but the babbling appears to be disappearing now. He responds to command with gestures. He has no interest in his musical toys, which disturbs his musician parents. Fine and gross motor skills, problem-solving skills, and psychosocial skills are all WNL.
Based on the above scenario, what could be the reason?
Answer
Deafness
Station 11. Case scenario - Burns
A 5-year child is caught in a house fire and brought to ER with 60% burns. His weight is around 16 kg. Answer the following questions.
- What is the most likely immediate complication likely to occur in this case and how will you identify this complication.
- What are the 4 most important steps in the management of this child?
- Write fluid therapy for the first 24 hours for this child?
Answers
- Airway obstruction & inhalational injury, (Singed nasal hairs, carbonaceous material in the throat, hoarseness of voice, persistent cough, stridor
- Air way management, BC, I/V access and fluids, Pain management, management of hypothermia
- Parkland formula (4 ml/kg/% burn) + Maintenance fluids
Case scenario 12. Case scenario - Foreign body
An asymptomatic 2 year old swallowed a hearing aid battery 4 hours previously. Chest x ray done after 4 hours at 11 PM showed battery located in the upper third of the esophagus. Child is playful and stable hemodynamically with no clinical symptomatology.
What will be the next step in your management and why?
Answer
Immediate esophagoscopy to retrieve the battery.
Why? - Hearing aid batteries are highly corrosive and must be removed as early as possible
Station 13. Case scenario - Fever with cough
A two-year-old child presents with fever, barking cough, and breathing difficulties. Initially, the child was having only a runny nose. On examination, tachypnoea, stridor, subcostal retractions, and intercostal retractions can be seen. Answer the following questions.
- What is the diagnosis?
- What is the usual etiological agent?
- Which X-ray sign is diagnostic of this condition
Answers
- Croup
- Parainfluenza A
- Steeple sign

Station 14. Case scenario - Tachypneic infant
Two yr old male child is brought to a health care center with complaints of a respiratory rate of 40/min without any chest indrawing. Answer the following questions.
- Classify the severity of the disease according to IMNCI.
- What is the choice of antibiotics?
Answers
- Severe pneumonia
- Amoxycillin and Septran
Bit of a theory
| Signs | Classification | Treatment |
|---|---|---|
| Any general danger signs or Chest indrawing or Stridor in a calm child. | Severe pneumonia | Give first dose of injectable chloramphenicol ( If not possible give oral amoxicillin). Refer URGENTLY to hospital. |
| Fast breathing | Pneumonia | Give Amoxycillin for 5 days. Soothe the throat and relieve the cough with a safe remedy if child is 6 months or older. Advise mother when to return immediately. Follow-up in 2 days. |
| No signs of pneumonia or very severe disease | No pneumonia / Cough or cold | If coughing for more than 30 days, refer for assessment. Soothe the throat and relieve the cough with a safe home remedy if a child is 6 months or older. Advise mother when to return immediately. Follow-up in 5 days if not improving. |
Station15. Case scenario - Mental retardation
A child has been diagnosed with mental retardation-
- How will you determine the degree of retardation and what are the different ranges
- What are the common causes you will look for
Answer
The DSM-IV classifies mental retardation into four stages based on severity:
- Mild (IQ score of 50-55 to approximately 70),
- Moderate (IQ score of 30-35 to 50-55),
- Severe (IQ score of 20-25 to 35-40), and
- Profound (IQ score of less than 20-25).
Station 16. Clinical case scenario - Ear pain and chronic discharge
A 5-year-old presented with chronic ear pain, and discharge from the left year for more than 3 week. ENT examination reveals perforated tympanic members. Answer the following question.
- What is the possible diagnosis?
- What are the differences between safe and unsafe CSOM?
- How would you treat safe and unsafe CSOM?
Answers
1. Chronic suppurative otitis media
2. Difference between safe and unsafe CSOM
| Safe CSOM | Unsafe CSOM |
|---|---|
| Tubotympanic disease | Atticoantral |
| central perforation | perforation in the attic |
| copious discharge | Scanty discharge |
| granulation absent | granulation common |
| No Cholesteatoma | cholesteatoma formed with the destruction of the mastoid bone |
| Conductive hearing loss | Mixed hearing loss |
3. Tympanoplasty is performed in safe CSOM while Mastoidectomy is performed in unsafe.
Station 17. Picture based diagnosis - Lump
Following is the clinical photograph of a 2-year-old boy who presented with an abdominal lump. Answer following question

- What is the likely Diagnosis
- How to treat?
- What is the prognosis?
Answers
- Neuroblastoma stage IV
- Chemotherapy, local surgery + radiotherapy, Autologous BMT, Cis retinoic Acid
- Poor prognosis. <30% chance of cure
Station 18. Picture based diagnosis - PS
Identify the cell shown in the peripheral smear

- Identify the cell
- Describe the neurological findings that may be observed in this condition
- Name the urinary investigation in this condition
Answers
1. Hypersegmented neutrophil (>5 lobes)
2. Neurological findings
– Paraesthesias
– Impaired position and vibration sense
– Ataxia
– Hyper or hyporeflexia
– Positive Babinski sign
3. Excessive excretion of methyl-malonic acid in urine is a sensitive index of Vit B12 deficiency
Station 19. Picture-based diagnosis - PS
Take a look at the following peripheral smear slide and answer the questions.

- Identify the cell
- Describe the characteristic feature of the cells in the smear.
- What is the diagnosis based on cell shown?
- Name 2 special stains which can aid in diagnosis.
Answers
1. Blast cell
2. Characteristics of cell
- Increased nuclear/cytoplasmic ratio
- Dense chromatin
- Pale cytoplasm
3. ALL L1
4. Sudan Black, NSE, MPO
Station 20. Clinical skills
What is the age group at which the following postural reflexes will appear or disappear?
- STNR
- ATNR
- Neck righting reflex
Answer
Here is a detailed guide on various postural and neonatal reflexes, including age on onset and age of disappearance.
Station 21. Clinical skill OSCE
What is the grade of asthma severity in a child having
- Symptoms of airflow obstruction > once a day.
- Night time symptoms > once a week.
- PEF – 60-80% of personal best with >30% of diurnal variation.
Answers
Moderate persistent asthma
Station 22. Developmental station
Fill in the following table regarding developmental reflexes in normal children
| Reflex | Age of Appearance | Age of disappearance |
| Rooting | ||
| Moro | ||
| Landau | ||
| Parachute |
Answers
| Reflex | Age of Appearance | Age of disappearance |
| Rooting | Birth | 3 months |
| Moro | Birth | 5-6 months |
| Landau | 10 months | 24 months |
| Parachute | 8-9 months | Persists |
Station 23. Genetics
Interpret the pedigree chart and answer the following questions.

- Identify the pattern of inheritance in the given Pedigree with an explanation.
- What is the basic reason for such an inheritance pattern?
- Give 2 more examples of similar inheritance?
Answer
- Mitochondrial inheritance. All the offspring born to an affected female are affected. Affected Males do not pass on the disease
- Because sperms don’t contain mitochondria, they can not pass the disease to offspring.
- Leigh disease and MELAS (Mitochondrial Encephalopathy with Lactic Acidosis and Stroke-like syndromes) also show mitochondrial inheritance.